Peripheral Arterial Disease (PAD)
Definition and Facts
 The term Peripheral Arterial Disease (PAD) or Peripheral Vascular Disease (PVD), is an occlusion or narrowing by atherosclerotic plaques of the arteries, not in the heart or brain. This means that the blood circulation through the arteries (large blood vessels that carry the blood from the heart) is decreased. This causes symptoms, most notably tight, aching, or squeezing pain in your calf, thigh, or buttock. This pain, called intermittent claudication, usually happens after you have walked a certain distance.
The term Peripheral Arterial Disease (PAD) or Peripheral Vascular Disease (PVD), is an occlusion or narrowing by atherosclerotic plaques of the arteries, not in the heart or brain. This means that the blood circulation through the arteries (large blood vessels that carry the blood from the heart) is decreased. This causes symptoms, most notably tight, aching, or squeezing pain in your calf, thigh, or buttock. This pain, called intermittent claudication, usually happens after you have walked a certain distance.
What is Peripheral Arterial Disease (PAD) or Peripheral Vascular Disease (PVD)?
Peripheral Arterial Disease (PAD) or Peripheral Vascular Disease (PVD) is a blood circulation disorder that causes the blood vessels outside of your heart and brain to narrow, block, or spasm. This can happen in your arteries or veins. PAD or PVD typically causes pain and fatigue, often in your legs, and especially during exercise. The pain usually improves with rest.
Are Atherosclerosis and Peripheral Arterial Disease (PAD) related?
There are two ways atherosclerosis causes disease;
- Atherosclerosis can limit the ability of the narrowed arteries to increase delivery of blood and oxygen to tissues during periods of increased oxygen demand such as during exertion, or
- Complete obstruction of an artery by a thrombus or embolus (thrombus and embolus are forms of blood clots; see below) resulting in tissue necrosis (death of tissue).
What are the signs and symptoms of Peripheral Arterial Disease (PAD)?
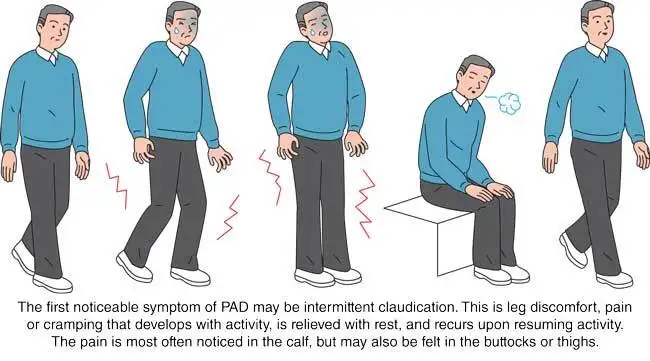
The first noticeable symptom of PAD may be intermittent claudication. This is leg discomfort, pain or cramping that develops with activity, is relieved with rest, and recurs upon resuming activity. The pain is most often noticed in the calf, but may also be felt in the buttocks or thighs.
Who is at risk for Peripheral Arterial Disease (PAD)?
About 5% of people over the age of 50 are believed to suffer from peripheral artery disease. This translates to about 10 million adults affected in the U.S. Peripheral artery disease affects men and women over the age of 50, with men having a slightly higher risk. The risk factors are associated with the same risk factors for development of atherosclerosis and coronary artery disease. Risk factors for peripheral artery disease include;
- High blood levels of the “bad” LDL cholesterol and triglycerides
- Low blood levels of the “good” HDL cholesterol
- Cigarette smoking
- Diabetes mellitus (both type 1 and type 2 diabetes)
- High blood pressure (hypertension) or a family history of hypertension
- A family history of atherosclerotic disease
- Chronic renal failure
- Overweight or obesity
- Physical inactivity
With peripheral artery disease, the risk factor is additive, meaning that a person with two risk factors – diabetes and smoking, for instance – has an increased chance of developing a severe case of peripheral artery disease than a person that only has one risk factor.
What tests are used to diagnose Peripheral Arterial Disease (PAD)?
The best way to see if you might have PAD is to get a complete checkup with your doctor. During a physical exam the doctor may look for signs of vascular disease and PAD, which might include a change in blood pressure in the limbs at rest and/or during a treadmill test, weak or absent artery pulse in the extremities, and skin color and nail changes. A vascular surgeon will also perform a physical exam. Your doctor may order certain tests to help diagnose PAD and determine the severity of the peripheral vascular disease.
- The ankle-brachial index (ABI) is a measurement of the blood pressure in the lower legs compared to the blood pressure in the arms. During this test, blood pressure cuffs are placed on the arms and legs. The cuffs are inflated, while a hand-held device (called a Doppler) is used to listen to the blood flow. In patients with significant peripheral artery disease in the legs, the blood pressures in the ankles will be lower than the blood pressure in the arms (brachial blood pressure). The ankle-brachial index ABI screening helps evaluate the amount of blood flow to the legs and feet, which is decreased in a person with PAD. It is a highly accurate method for detecting PAD.
- Typically an angiogram is done to determine where the peripheral artery plaque has built up so treatment options can be assessed. This can be done using a CT or MRI, or possibly by doing a catheter-directed angiogram, which involves placing a thin tube into the artery and injecting dye into the arteries to see where the blockages are located.
- A pulse volume recording (PVR) is a noninvasive test that measures the blood volume changes that occur in the legs. During this test, a blood pressure cuff is placed on the arm, and multiple cuffs are placed on the legs. The cuffs are inflated slightly while the patient is lying down. As blood pulses through the arteries, the blood vessels expand, causing an increase or decrease in the volume of air within the cuff. A recording device displays these pulse volume changes as a waveform on a monitor. Blood pressures are measured before and after exercise on a treadmill and help define if the pain is due to PAD or other causes. The PVR test also helps locate the area of blockages in the extremity of the legs.
- A vascular ultrasound is a noninvasive test used to examine blood circulation. During a vascular ultrasound, a transducer (small hand-held device) is placed on the skin over the artery to be examined. The transducer emits sound waves that bounce off the artery. These sound waves are recorded, and an image of the vessel is created and displayed on a monitor. This test may be used to detect a blockage in an artery.
What are the management and treatment guidelines for Peripheral Arterial Disease (PAD)?
The American College of Cardiology Foundation and the American Heart Foundation (ACCF/AHA) collaborated to create the “2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Peripheral Artery Disease (Updating the 2005 Guideline).” You can read the published document here.
They recommend the following lifestyle changes:
- Regular physical activity – Your doctor will recommend an effective treatment of supervised exercise training. The patient may have to start slowly and progress to a goal set by the doctor. Decreased symptoms of vascular disease can be achieved in just 4-8 weeks by following a simple regimen three times a week of walking, leg exercises, and a treadmill program. Walking might be painful starting out as intermittent claudication (pain in calves and thighs) may call for a program of alternating between activity and resting
- Diet changes and adjustments – If you are an individual with PAD, you may also have elevated cholesterol levels. A diet low in saturated fat, trans fat, and cholesterol, as well as plenty of fruit and vegetables, can help lower blood cholesterol levels.
- Smoking cessation – Quitting smoking reduces symptoms and lowers your chance of having your peripheral artery disease (and arteries elsewhere) get worse.
- Some medications – the doctor may prescribe antihypertensive drugs as well as statins to lower cholesterol levels.
Surgery to treat Peripheral Arterial Disease (PAD)
PAD may be treated in the San Antonio Regional Hospital Cardiac Catheterization Lab by interventional cardiologists. Balloon angioplasty, also known as percutaneous transluminal angioplasty, or PTA, is a nonsurgical procedure that can widen a narrowed or blocked artery. Using imaging for guidance, the cardiologists thread a catheter through the femoral artery in the groin, to the blocked artery in the legs. Then a balloon is inflated to open the blood vessel where it is narrowed or blocked. In some cases, this is then held open with a stent, (a cylindrical wire mesh tube). Angioplasty does not require general anesthesia. Usually, a local anesthetic at the area of catheter insertion and a mild sedative is given.
What are the potential complications of Peripheral Arterial Disease (PAD)?
Complications from undiagnosed and untreated vascular disease can be serious and even life-threatening. Restricted blood flow of PAD can be a warning sign of other forms of vascular disease. Complications of PAD can include:
- tissue death, which can lead to extremity limb amputation
- impotence
- pale skin
- pain at rest and with movement (claudication)
- severe arm or leg pain that restricts mobility
- non-healing wounds
- coronary artery heart disease (vascular disease)
- life-threatening infections of the bones and bloodstream
- blood clots
The most serious complications involve the arteries bringing blood to the heart and brain. When these become clogged, it can lead to heart attack, stroke, or death.
How can I prevent Peripheral Arterial Disease (PAD)?
Addressing the following risk factors can help prevent or delay PAD:
- Smoking – smoking is more closely related to developing heart disease than any other risk factor. Regular smokers are four times as likely to develop PAD than lifetime non-smokers. Talk to a doctor about programs and products that can help you quit smoking.
- Diet – follow a healthy eating plan that is low in total fat, saturated fat, trans fat, cholesterol, and sodium. Eat plenty of fruits, vegetables, and low-fat dairy products. Overweight and obese patients should work with a doctor to create a reasonable weight-loss plan. If you have diabetes, controlling high blood sugar can prevent damage to blood vessels.
- Exercise – Regular exercise, such as walking, can reduce symptoms and increase the distance you can walk without symptoms.
- Maintain a healthy weight.
- Follow your health-care professional’s recommendations for controlling high blood pressure and high cholesterol.
Treatment
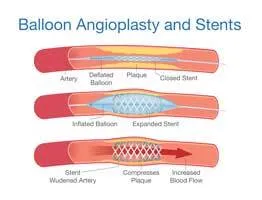
PAD may be treated in the San Antonio Regional Hospital Cath Lab by interventional cardiologists. Using imaging for guidance, the cardiologists thread a catheter through the femoral artery in the groin, to the blocked artery in the legs. Then a balloon is inflated to open the blood vessel where it is narrowed or blocked. In some cases, this is then held open with a stent, a tiny metal cylinder. This is a minimally invasive treatment that does not require surgery, just a small opening in the skin about the size of a pencil tip.
Balloon angioplasty and stenting have generally replaced invasive surgery as the first-line treatment for PAD. Studies have shown interventional therapy for PAD to be as effective as surgery for many arterial occlusions.
Heart Institute Quick Links
- Healthgrades™ 50 Best Award
- 2022 Cardiac Workshops
- 2020 Cardiac Workshops
- 2019 Cardiac Workshops
- Balloon Angioplasty
- Cardiac Arrhythmia Surgery
- Cardiac Catheterization
- Cardiac Educational Classes
- Cardiac Rehabilitation
- Cardiac Rehabilitation Outpatient
- Cardiovascular Surgery
- Coronary Artery Bypass Graft
- Coronary Artery Disease
- Coronary Artery Disease Diagnostic Testing
- ECMO
- Electrophysiology
- Heart and Cardiovascular Surgery
- Heart Rhythms Arrhythmias
- Heart Valve Repair
- Impella Left Ventricular Assist Device
- Implantable Cardioverter Defibrillator
- Off-Pump Coronary Bypass Surgery
- Pacemaker
- Peripheral Arterial Disease
- Stent Placement
- Supraventricular Tachycardia
- Transcatheter Aortic Valve Replacement (TAVR)
- Valve Disease
- Wolff Parkinson White Syndrome
